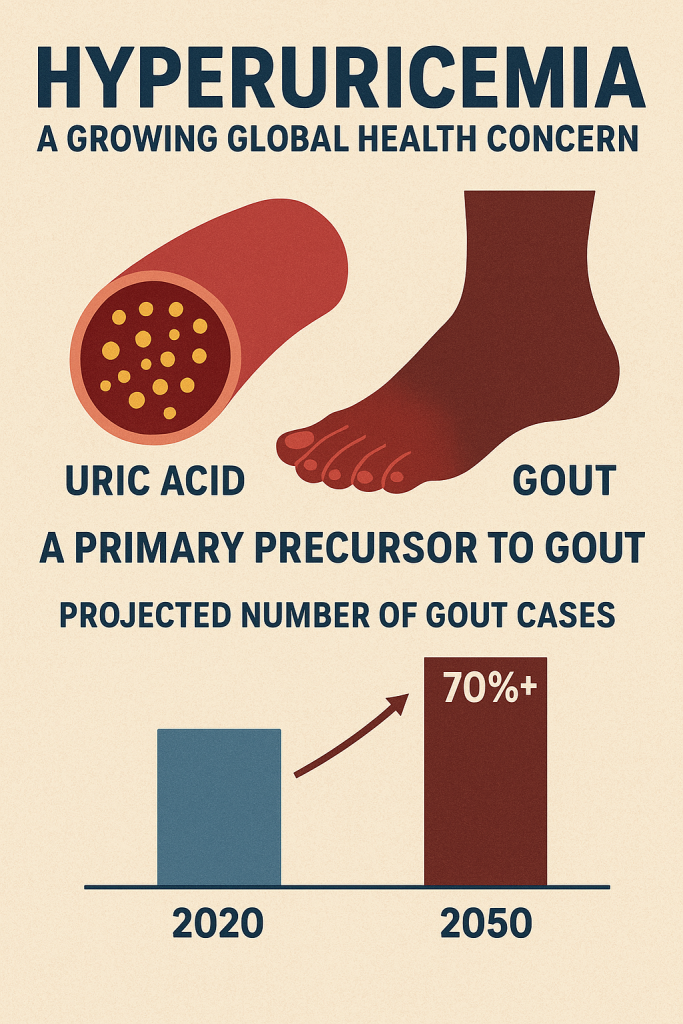
A growing global health concern, hyperuricemia—an excess of uric acid in the blood—affects millions and is a primary precursor to gout, a debilitating form of inflammatory arthritis.[1] Despite its prevalence, long-term management remains a significant challenge, with a large portion of patients failing to achieve target uric acid levels. A 2024 study in The Lancet Rheumatology forecasts that the number of individuals with gout will surge by over 70% between 2020 and 2050, primarily driven by population growth and aging.[2][3][4] This projection highlights the urgent need for a deeper understanding of the condition’s complex physiology and the persistent gaps in treatment.
The Complex Nature of Uric Acid Metabolism
Uric acid is the final product of purine metabolism in humans.[5][6][7] Its levels are determined by a delicate balance between production and excretion. However, this balance is more complex than it appears:
- Internal Production Dominates: Approximately two-thirds of the body’s uric acid is produced endogenously (internally) from the natural breakdown of cells, while only about one-third comes from exogenous sources, such as the digestion of purine-rich foods.[5][8] This intrinsic metabolic reality means that for many, dietary restrictions alone are insufficient for managing high uric acid levels.[9]
- Kidney Excretion is Key: The kidneys are responsible for eliminating about 70% of the body’s daily uric acid production.[5] Therefore, any impairment in renal function can lead to an accumulation of uric acid. Up to 90% of hyperuricemia cases are caused by reduced renal excretion rather than overproduction.[10][11]
- Genetic Predisposition: Genetics plays a substantial role in how the body metabolizes and excretes uric acid.[11][12] Genes such as SLC2A9 and ABCG2, which code for proteins that transport urate in the kidneys, are major regulators.[10][13] Variations in these genes can significantly increase an individual’s risk for developing hyperuricemia and gout, a reality that cannot be reversed with current single-therapy treatments.[10][12][13]
Furthermore, factors like aging, which naturally decreases kidney efficiency, and the presence of comorbidities like obesity, diabetes, and hypertension, complicate treatment and are themselves difficult to manage.[14]
A Public Health Challenge Fueled by Global Trends
The burden of gout is substantial and appears to be growing worldwide, particularly in developed nations.[15] This trend is closely linked to rising rates of obesity, dietary shifts, and an aging population.[2][4]
- Global Prevalence: In 2020, an estimated 55.8 million people worldwide had gout.[2][16][17] Projections suggest this number will climb to nearly 96 million by 2050.[2][16][18]
- Demographic Disparities: Gout disproportionately affects men, who had a prevalence rate over three times higher than women in 2020.[2][4][16] Prevalence also rises sharply with age.[2][19]
- Regional Differences: High-income regions like North America and Australasia report some of the highest prevalence rates.[17] The significant increase in these areas since 1990 underscores the impact of lifestyle and environmental factors on top of genetic susceptibility.[17]
Limitations and Pitfalls of Traditional Therapies
Conventional medical treatments for hyperuricemia, while effective at lowering uric acid levels, are not without significant limitations and potential risks.
Commonly prescribed medications like allopurinol and febuxostat work by inhibiting xanthine oxidase, an enzyme essential for uric acid production.[20] However, they do not address the root cause of metabolic dysfunction and can have serious side effects:
- Allopurinol can cause side effects ranging from rash and fever to more severe issues like hepatitis and kidney problems.[20][21]
- Febuxostat carries a black box warning from the U.S. FDA due to an increased risk of cardiovascular-related death compared to allopurinol.[21][22][23] Other potential side effects include rash, nausea, and impaired liver function.[21][24]
- Benzbromarone, another frontline medication, has been withdrawn from the European market due to concerns about severe liver toxicity.
Common therapeutic missteps can also undermine treatment. Some patients who start with a high dose of medication to rapidly lower uric acid may trigger acute gout attacks, a phenomenon known as “dissolution pain.”[20][22] Conversely, an over-reliance on strict, often misguided, dietary restrictions can lead to nutritional deficiencies without effectively controlling uric acid levels.[9]
Widespread Gaps in Gout Management
Globally, the management of gout is frequently suboptimal, with a significant gap between clinical guidelines and real-world practice.[25][26][27] Many patients do not receive urate-lowering therapy, and of those who do, adherence is often poor.[26][27]
Studies from around the world paint a concerning picture:
- In the United States, less than two-thirds of gout patients were estimated to be using urate-lowering therapy in 2019.[27]
- Systematic reviews have consistently identified significant knowledge gaps among primary care physicians, which contributes to inadequate patient education about the chronic nature of the disease.[25]
This lack of specialized care and patient understanding allows the disease to progress, leading to a dangerous cycle of complications.
The Vicious Cycle of Hyperuricemia and Kidney Disease
The relationship between high uric acid and kidney disease is a two-way street. Excess uric acid can crystallize in the urinary tract, forming kidney stones and causing chronic interstitial nephritis, which impairs kidney function.[28][29]
As kidney function declines, the body’s ability to excrete uric acid is further compromised, causing uric acid levels to rise even higher.[28][30] This creates a vicious cycle that accelerates the progression of chronic kidney disease (CKD), making the management of hyperuricemia even more challenging.[28]
The Future of Treatment: A Multi-faceted Approach
Recognizing the limitations of current treatments, researchers are exploring therapies that target the three core pathways of gout pathology: uric acid overproduction, inadequate excretion, and the resulting inflammatory response.
A growing area of interest is the use of natural compounds to manage uric acid without the harsh side effects of pharmaceuticals. For example, the BISPIT 3310 series is based on this multi-pathway approach. It incorporates ingredients like:
- Celery Seed Extract: Studies in rodents suggest that compounds in celery seed, such as luteolin, may help lower uric acid levels by inhibiting xanthine oxidase and provide anti-inflammatory and antioxidant effects.[31][32][33][34]
- Himalayan White Thorn Plant Salt: This ingredient is believed to promote the excretion of uric acid.
- High-Concentration Liquid Formulas: Designed to quickly counter the inflammatory response during an acute attack.
These natural approaches, which also include dietary choices like cherries and berries, aim to reduce the frequency of acute gouty arthritis episodes over the long term.[35][36][37][38]
Given the chronic nature of hyperuricemia, effective management requires a long-term commitment from patients. This includes regular monitoring of uric acid levels and kidney function, adherence to a sustainable management plan, and professional medical guidance to adjust strategies as needed. For now, a scientifically informed and proactive approach is the best defense against the pervasive challenge of high uric acid.
Sourceshelp
- biospace.com
- nih.gov
- hcplive.com
- thehansindia.com
- medscape.com
- nih.gov
- researchgate.net
- thegoutkiller.com
- nih.gov
- nih.gov
- oup.com
- gouteducation.org
- researchgate.net
- nih.gov
- semanticscholar.org
- johnshopkins.edu
- ahr4health.net
- csu.edu.au
- nih.gov
- goodrx.com
- mayoclinic.org
- healthline.com
- fda.gov
- versusarthritis.org
- nih.gov
- researchgate.net
- nih.gov
- nih.gov
- mdpi.com
- researchgate.net
- nih.gov
- healthline.com
- researchgate.net
- peoplespharmacy.com
- ebsco.com
- precisionrheum.com
- healthline.com
- arthritiscare.com.au
