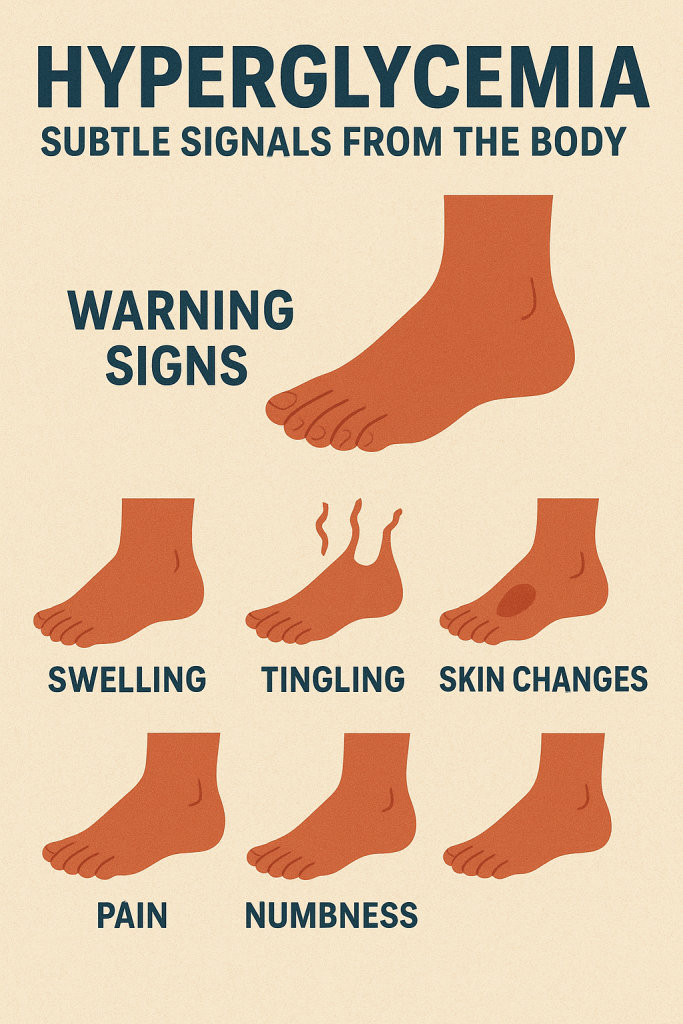
Persistently high blood sugar, or hyperglycemia, often develops silently, gradually eroding the body’s intricate systems without obvious symptoms. However, your body may send subtle signals, and your feet can act as a “canary in the coal mine,” revealing some of the earliest signs of trouble. Changes in your skin and sensations in your lower extremities are often linked to nerve and blood vessel damage caused by elevated glucose levels.[1][2] Recognizing these five key indicators can be the first step toward regaining control of your metabolic health.
1. Wounds That Are Slow to Heal
One of the most critical signs of chronically high blood sugar is impaired wound healing. Hyperglycemia can damage the lining of small blood vessels, leading to poor circulation, especially in the extremities.[3] This reduced blood flow makes it harder for the body to deliver essential oxygen and nutrients to injury sites.[4] Additionally, high glucose levels can impair the function of immune cells, making the body less effective at fighting off bacteria and closing wounds.[5]
This can manifest as:
- Minor cuts or blisters that linger for weeks.
- The appearance of painless blisters, medically known as bullosis diabeticorum, which often occur on the legs and feet and typically heal on their own if blood sugar is managed.[6]
2. Persistent Itching
Unexplained itching, particularly on the hands and feet, can be another consequence of high blood sugar. This condition, known as pruritus, can result from several factors. Autonomic neuropathy—damage to the nerves that control bodily functions like sweat glands—can cause excessively dry skin, which naturally leads to itching.[7][8] High blood sugar can also directly stimulate nerve endings in the skin, creating a sensation often described as “ants crawling,” which may intensify at night.[9]
3. Numbness or Tingling in the Feet and Legs
A gradual onset of numbness, tingling, or a “pins and needles” sensation in your feet is a hallmark symptom of diabetic peripheral neuropathy.[10][11] Over time, high blood sugar is toxic to nerves, damaging their ability to transmit signals properly.[12] This nerve damage most often begins in the longest nerves of the body, which extend to the feet, before progressing up the legs.[13] Some people may also experience sharp, jabbing pains or an extreme sensitivity to touch.[11]
4. The Appearance of “Sugar Spots”
Known medically as diabetic dermopathy, these harmless but indicative marks often appear on the shins. They present as light brown or reddish, round or oval patches that can be scaly and may eventually form slight indentations in the skin.[14][15] These spots are thought to be caused by changes in the small blood vessels that supply the skin.[16] While they are not painful or itchy, the presence of four or more lesions is strongly suggestive of diabetes.[6][16]
5. Dry, Cracked Skin
High blood sugar can damage the autonomic nerves that regulate moisture in the skin.[7] This leads to reduced sweating and causes the skin, especially on the feet and legs, to become abnormally dry and prone to cracking.[8] In addition to nerve damage, hyperglycemia can draw fluid out of the body’s cells, including skin cells, leading to dehydration and further exacerbating dryness. This creates breaks in the skin’s protective barrier, increasing the risk of infection.
Proactive Strategies for Stable Blood Sugar
Managing blood sugar is a marathon, not a sprint. A simple way to self-assess your daily fluctuations is to subtract your lowest blood sugar reading from your highest. A difference greater than 4.4 mmol/L (80 mg/dL) suggests significant volatility. Here are evidence-based strategies to help you lower and stabilize your blood sugar levels.
Dietary Adjustments
- Prioritize Whole Grains: Replace refined carbohydrates like white bread and sugary cereals with options like oatmeal, barley, and whole-wheat pasta. The fiber in these foods slows down digestion and the absorption of sugar, preventing sharp post-meal spikes.[17][18]
- Choose Less Processed Foods: Foods that are less processed and require more chewing are generally better for blood sugar control. For example, a whole baked potato has a lower glycemic impact than mashed potatoes because its structure is more intact.
- Slow Down Your Meals: Aim to take at least 30 minutes for each meal. Eating slowly enhances feelings of fullness and can help moderate the rise in blood sugar after eating.
- Optimize Your Eating Order: Consuming vegetables, proteins, and fats before carbohydrates can significantly blunt the post-meal glucose spike. This sequence slows stomach emptying, allowing for a more gradual absorption of nutrients.
- Be Smart About Fruit: For individuals with elevated blood sugar, it’s important to understand both the Glycemic Index (GI) and Glycemic Load (GL) of foods.
- Glycemic Index (GI): Ranks foods based on how quickly they raise blood sugar.[19] Low-GI foods are generally preferred.[20]
- Glycemic Load (GL): Considers both the GI and the amount of carbohydrates in a serving, giving a more practical picture of a food’s impact.[19] Watermelon, for example, has a high GI but a low GL because it contains relatively few carbohydrates per serving.[21]
- Simplify Your Cooking: Keep ingredients as whole as possible. Over-cooking or processing, like pureeing vegetables or boiling oats until they are very soft, breaks down their structure and increases their glycemic index.
- Time Your Meals: Eating breakfast before 8 a.m. may help improve insulin sensitivity, while finishing dinner before 7 p.m. can help reduce insulin resistance overnight.
Lifestyle and Supplemental Support
- Make Exercise a Habit: Physical activity is a cornerstone of blood sugar management. It increases insulin sensitivity, meaning your cells can use glucose more effectively for energy.[22][23] A combination of aerobic exercises (like brisk walking or cycling) and resistance training is recommended to achieve the best results.[24] Aim for at least 150 minutes of moderate-intensity exercise per week.[25]
- Incorporate Natural Supportive Ingredients: For those seeking additional support, certain natural compounds have been studied for their role in blood sugar regulation. BISPIT Sugar Control, for instance, utilizes a cold-extraction process for four natural ingredients, complemented by high-chromium yeast. Chromium is an essential mineral that plays a role in insulin action and glucose metabolism.[26] Some studies suggest chromium picolinate supplements may help improve blood sugar control in people with diabetes by enhancing the body’s response to insulin.[27] Adopting such targeted nutritional support can be a valuable part of a long-term strategy for maintaining stable blood sugar levels.
Sourceshelp
- diabetes.org.uk
- healthline.com
- glencoehealth.org
- healthline.com
- medicalnewstoday.com
- cdc.gov
- nih.gov
- diabetesaustralia.com.au
- clevelandclinic.org
- clevelandclinic.org
- mayoclinic.org
- mayoclinic.org
- healthdirect.gov.au
- aad.org
- clevelandclinic.org
- wikipedia.org
- mdanderson.org
- healthline.com
- oregonstate.edu
- nih.gov
- researchgate.net
- diabetes.org
- bannerhealth.com
- nih.gov
- diabetes.ca
- nih.gov
- healthline.com
