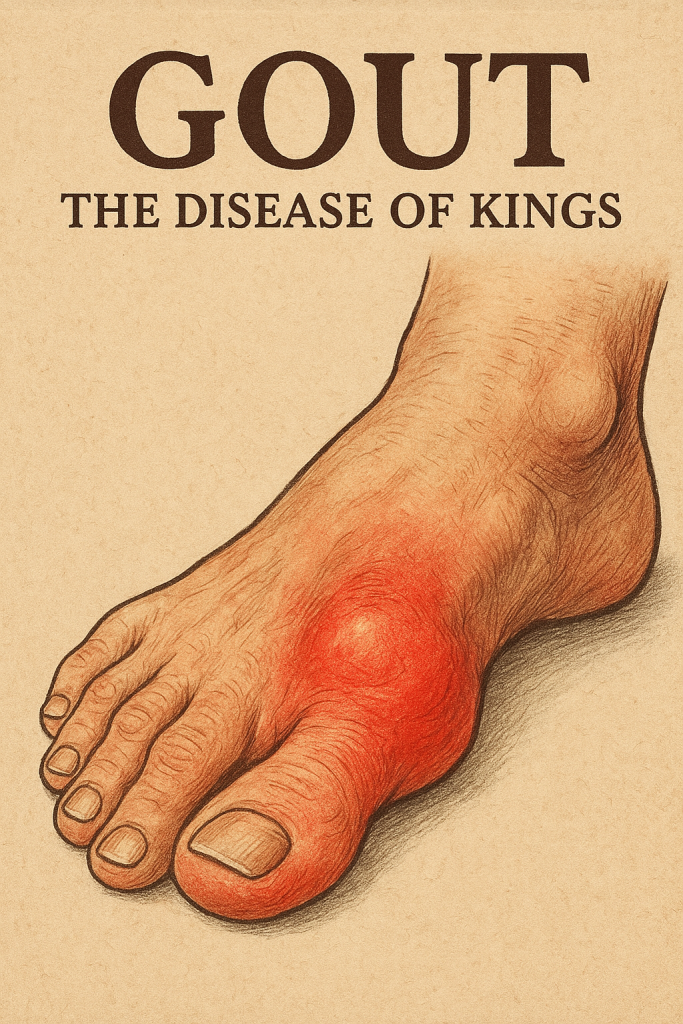
Gout, a condition once caricatured as the “disease of kings,” is a profoundly painful and often misunderstood form of inflammatory arthritis. Its signature is the sudden, excruciating onset of a flare-up—an attack of intense pain, swelling, redness, and heat in a joint, most famously the big toe. For those living with the condition, gout is far more than an occasional inconvenience; it is a chronic illness that can permeate every aspect of daily life, turning simple activities like walking, working, or even sleeping into monumental challenges.
However, a diagnosis of gout does not have to be a sentence to a life of pain and limitation. While there is no cure, gout is one of the most manageable forms of arthritis. The key to reclaiming control lies in a proactive, informed, and consistent approach to managing the underlying cause: high levels of uric acid in the blood, or hyperuricemia. This comprehensive guide is designed to empower individuals with gout by exploring how to navigate and adapt daily activities. From the crucial role of exercise and the subtleties of a gout-friendly diet to managing work, stress, and practical everyday considerations, this article will provide the framework for not just coping with gout, but thriving despite it.
Chapter 1: Understanding Gout’s Impact on Daily Life
To effectively manage gout, one must first appreciate the full scope of its impact. The condition manifests in different phases, each presenting unique challenges to daily routines, as outlined by rheumatology experts.
The Gout Flare: An Acute Disruption
The most dramatic and debilitating phase of gout is the acute flare or attack. It occurs when monosodium urate (MSU) crystals, which have formed in the joint due to sustained hyperuricemia, trigger a massive inflammatory response mediated by the innate immune system. The experience is often described as feeling like the joint is on fire or filled with shards of broken glass, with maximal pain often reached within 12-24 hours.
During a flare, daily activities grind to a halt. The simple act of a bedsheet touching an inflamed toe can be unbearable. Walking becomes impossible, requiring the use of crutches or complete bed rest. Simple tasks such as showering, dressing, or preparing a meal become Herculean efforts. This period, which can last for days or even weeks if untreated, is a stark reminder of the condition’s severity and serves as a powerful motivator for long-term management.
The Intercritical Period: The Crucial Window for Management
Following a flare, there is a symptom-free period known as the intercritical period. It is tempting to believe the problem has gone away, but this is a dangerous misconception. The underlying hyperuricemia persists. MSU crystals may still be silently depositing in the joints and soft tissues, setting the stage for the next attack and causing slow, progressive joint damage, a process visible on advanced imaging even in the absence of symptoms.
This is the most critical time for proactive, long-term urate-lowering therapy and lifestyle modification. The choices made during this phase will determine the frequency and severity of future flares and prevent the progression to chronic disease.
Chronic Tophaceous Gout: The Consequence of Inaction
If gout is left unmanaged or poorly managed over many years, it can progress to a chronic and deforming stage. Urate crystals can accumulate into large deposits called tophi (singular: tophus). These are chalky, white nodules that form under the skin, in and around joints, in bursae, and along tendons.
Tophi are not just a cosmetic issue. They are active sites of inflammation that can cause persistent stiffness, chronic pain, and severe joint erosion, leading to permanent disability and a significant reduction in quality of life. At this stage, gout’s impact on daily activities is no longer intermittent but constant.
The Psychological Toll
The impact of gout extends beyond the physical. The unpredictable nature of the flares can lead to significant anxiety and fear. Studies have shown that patients with gout report high levels of functional disability and a lower health-related quality of life compared to the general population. The chronic pain and physical limitations can also lead to a higher prevalence of depression. Addressing the mental and emotional aspects of living with gout is a vital part of a holistic management plan.
Chapter 2: The Cornerstone of Gout Management: Exercise and Physical Activity
Regular, appropriate physical activity is one of the most powerful tools for managing the condition between flares.
Why Exercise is Crucial for Gout
The benefits of exercise for individuals with gout are multi-faceted and supported by clinical evidence:
- Weight Management: There is a strong, dose-dependent relationship between BMI and serum uric acid levels. Obesity is a major risk factor for developing gout. Losing weight through diet and exercise can dramatically lower serum uric acid levels and reduce the frequency of gout attacks.
- Improving Joint Health: Movement helps maintain the flexibility and range of motion of joints. It also strengthens periarticular muscles, which provide better support and stability, reducing mechanical stress on the joint cartilage that gout can damage.
- Reducing Systemic Inflammation: Regular moderate exercise has a proven systemic anti-inflammatory effect, which may help create a less favorable environment for flares to occur.
- Managing Co-morbidities: Gout is closely associated with metabolic syndrome, including hypertension, dyslipidemia, insulin resistance, and cardiovascular disease. Exercise is a first-line, non-pharmacological treatment for these co-morbidities, making it essential for improving overall health and reducing cardiovascular risk in patients with gout.
Exercising During a Gout Flare: What You Should and Shouldn’t Do
During an acute attack, the inflamed joint must be protected.
- The “Don’t” List: Do not exercise the affected joint. This will intensify the inflammatory response, prolong the attack, and risk further damage to the articular cartilage.
- The “Do” List: The focus should be on the R.I.C.E. method: Rest, Ice, Compression, and Elevation. Rest the joint completely. Apply ice packs to reduce swelling and pain. While the affected joint is resting, performing gentle range-of-motion exercises for unaffected joints is encouraged to prevent deconditioning.
Exercising Between Gout Flares: A Detailed Action Plan
During the intercritical, pain-free periods, a consistent exercise routine should be a priority, focusing on joint-friendly activities.
- Low-Impact Aerobic Activities: These activities raise your heart rate without jarring the joints.
- Swimming and Water Aerobics: The buoyancy of water supports body weight, making this an ideal exercise for people with arthritis of the lower extremities.
- Cycling: Excellent for cardiovascular health and strengthening leg muscles with minimal joint impact.
- Walking: A highly effective and accessible form of exercise. Proper footwear is essential.
- Elliptical Trainer: Simulates running without the associated high-impact forces.
- Strength Training: The American College of Rheumatology strongly recommends strength training for individuals with arthritis to improve muscle function and reduce pain. Focus on proper form with resistance bands, light weights, or machines.
- Flexibility and Range of Motion: Activities like Tai Chi and Yoga are recommended for improving balance, flexibility, and physical function in people with arthritis.
Creating Your Routine:
- Start Low, Go Slow: This principle is crucial to avoid injury or triggering a flare.
- Hydrate: Dehydration can increase serum urate concentration and is a known trigger for gout flares. It is vital to drink water before, during, and after exercise.
- Consult a Professional: The 2020 American College of Rheumatology Guideline for the Management of Gout recommends a treat-to-target strategy, which should be managed by a physician. Always discuss exercise plans with your doctor or a physical therapist.
Chapter 3: Navigating Work and Professional Life with Gout
Gout can significantly interfere with work productivity and attendance, a concept known as presenteeism and absenteeism.
Adapting Your Workspace
- For Desk Jobs: Take regular breaks to stand and move. An ergonomic setup, including a supportive chair and footrest, can reduce strain.
- For Physically Demanding Jobs: Discuss potential accommodations under workplace disability guidelines. This can include ergonomic adjustments, task modification, or enhanced break schedules. Proper, supportive footwear is non-negotiable.
Managing Gout Flares at Work
- The Gout Emergency Kit: Keeping prescribed anti-inflammatory medication (e.g., NSAIDs, colchicine) on hand to be taken at the very first sign of a flare is a key management strategy recommended by clinical guidelines. Early initiation of treatment drastically improves outcomes.
- Communication: Informing your supervisor or HR about your condition can facilitate necessary accommodations and foster a supportive environment.
Chapter 4: The Role of Diet and Hydration in Daily Routine
Dietary and lifestyle modifications are recommended as an adjunct to, not a replacement for, urate-lowering medication for all patients with gout.
Structuring Your Day for a Gout-Friendly Diet
- Limit High-Purine Foods: The strongest recommendations are for limiting alcohol (especially beer), purine-rich meats (organ meats, red meat), and high-fructose corn syrup.
- Encourage Beneficial Foods: Evidence supports the consumption of low-fat dairy products, which have been shown to have a urate-lowering effect. Some studies suggest that cherry consumption is associated with a lower risk of gout attacks, potentially due to their anti-inflammatory properties.
- Focus on a Healthy Pattern: A balanced, heart-healthy diet like the DASH diet (Dietary Approaches to Stop Hypertension), which is rich in fruits, vegetables, and low-fat dairy, has been shown to lower serum uric acid levels.
Hydration as a Constant Activity
Adequate water intake helps the kidneys excrete uric acid and prevents the dehydration that can trigger flares.
Chapter 5: Footwear, Clothing, and Other Practical Daily Considerations
The podagra, or inflammation of the first metatarsophalangeal joint (the big toe), is the initial symptom in about 50% of gout cases. This makes footwear a critical daily consideration.
- The Primacy of Proper Footwear: Shoes should have a wide toe box to avoid compressing the joint, good arch support, and excellent cushioning to absorb shock. During a flare, open-toed or adjustable footwear may be necessary.
- Clothing and Bedding: Loose-fitting clothing and the use of a bed cradle to keep sheets off an inflamed joint can significantly improve comfort during a flare.
Chapter 6: Stress Management and Mental Well-being
While the direct link is still being researched, many patients report that high levels of physical or emotional stress can trigger their gout flares.
Daily Stress-Reduction Techniques
- Mindfulness and Exercise: Mind-body practices like mindfulness meditation and regular physical activity are proven methods for reducing stress and improving the psychological well-being of patients with chronic diseases.
- Patient Education and Support: Understanding the condition is key to reducing anxiety. The American College of Rheumatology guidelines emphasize the importance of patient education. Support groups like those found through the Arthritis Foundation can provide validation and coping strategies.
Conclusion: Taking Control and Living Fully
Gout is a serious, chronic disease, but it is not unmanageable. The current “treat-to-target” approach, which aims to lower and maintain serum uric acid below 6 mg/dL, can effectively eliminate flares and resolve tophi over time. This requires a partnership between the patient and physician, combining long-term urate-lowering therapy with a daily commitment to a healthy lifestyle. By embracing joint-friendly exercise, a balanced diet, and proactive stress management, individuals with gout can dramatically reduce the condition’s impact and continue to engage in the daily activities that bring you joy and fulfillment.
References
- FitzGerald, J. D., Dalbeth, N., Mikuls, T., et al. (2020). 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis & Rheumatology, 72(6), 879–895. https://doi.org/10.1002/art.41247
- Dalbeth, N., Merriman, T. R., & Stamp, L. K. (2016). Gout. The Lancet, 388(10055), 2039–2052. https://doi.org/10.1016/S0140-6736(16)00346-9
- Ragab, G., Elshahaly, M., & Bardin, T. (2017). Gout: An old disease in new perspective – A review. Journal of Advanced Research, 8(5), 495–511. https://doi.org/10.1016/j.jare.2017.04.008
- Richette, P., & Bardin, T. (2010). Gout. The Lancet, 375(9711), 318–328.
- Perez-Ruiz, F., Dalbeth, N., & Bardin, T. (2015). A review of uric acid, crystal deposition disease, and gout. Advances in Therapy, 32(1), 31–41.
- Becker, M. A., Schumacher, H. R., Benjamin, K. L., et al. (2009). Quality of life and disability in patients with chronic gout. Journal of Rheumatology, 36(5), 1041-1048.
- Choi, H. K., Atkinson, K., Karlson, E. W., & Curhan, G. (2004). Obesity, weight change, and risk of gout in men: the Health Professionals Follow-up Study. Archives of Internal Medicine, 164(7), 742–748.
- Choi, H. K., Atkinson, K., Karlson, E. W., et al. (2004). Purine-rich foods, dairy and protein intake, and the risk of gout in men. New England Journal of Medicine, 350(11), 1093–1103. https://www.nejm.org/doi/full/10.1056/nejmoa035700
- Zhang, Y., Neogi, T., Chen, C., et al. (2022). Cherry consumption and the risk of recurrent gout attacks. Arthritis & Rheumatism, 64(12), 4004–4011. https://doi.org/10.1002/art.34677
