Introduction
When struggling with brain fog, irritability, or persistent mood swings, we often look to psychological stress or neurological issues as the primary culprits. However, an increasing body of clinical evidence suggests that our emotional and cognitive states are profoundly linked to the health of our liver. Chronic Liver Disease (CLD) can disrupt central nervous system function through a complex network of physiological pathways, making your liver’s health a critical factor in your mental well-being.
I. Physiological Mechanisms: The Liver-Brain Axis
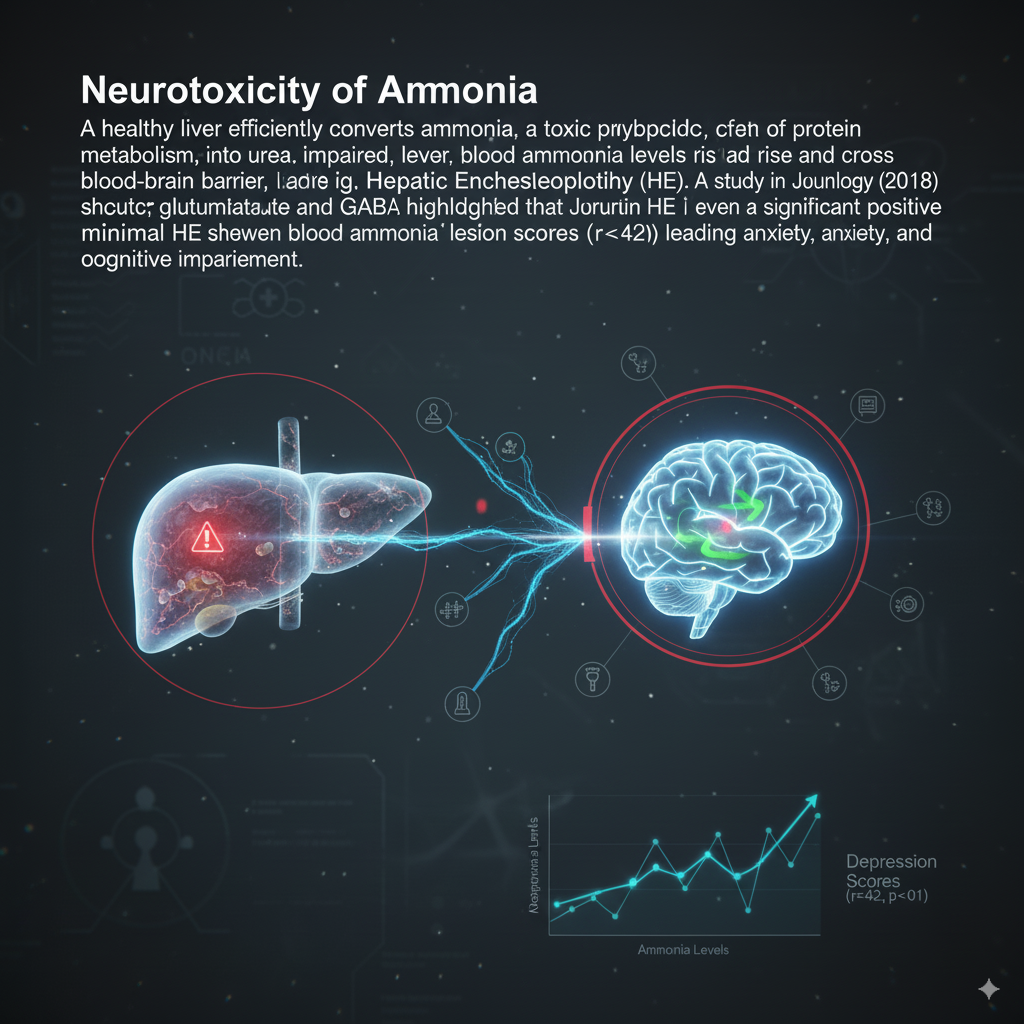
- Neurotoxicity of Ammonia
A healthy liver efficiently converts ammonia, a toxic byproduct of protein metabolism, into urea. When liver function is impaired, blood ammonia levels rise and cross the blood-brain barrier, leading to Hepatic Encephalopathy (HE). In the brain, ammonia disrupts neurotransmitter balance, particularly glutamate and GABA. A study in the Journal of Hepatology (2018) highlighted that even minimal HE shows a significant positive correlation between blood ammonia levels and depression scores (r=0.42, p<0.01), leading to anxiety, apathy, and cognitive impairment.
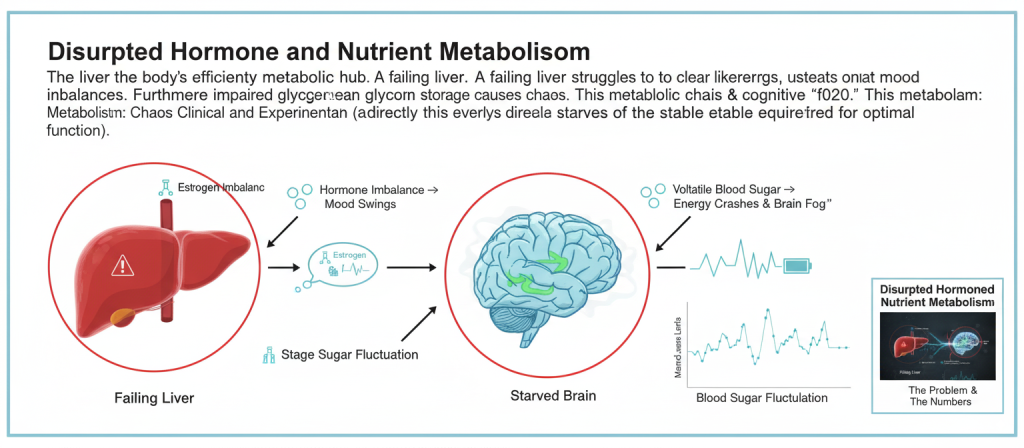
- Disrupted Hormone and Nutrient Metabolism
The liver is the body’s primary metabolic hub. A failing liver struggles to clear hormones like estrogen, leading to imbalances that can manifest as mood swings. Furthermore, impaired glycogen storage causes volatile blood sugar, leading to energy crashes and cognitive “fog.” This metabolic chaos, documented in Metabolism: Clinical and Experimental (2020), directly starves the brain of the stable energy required for optimal function.
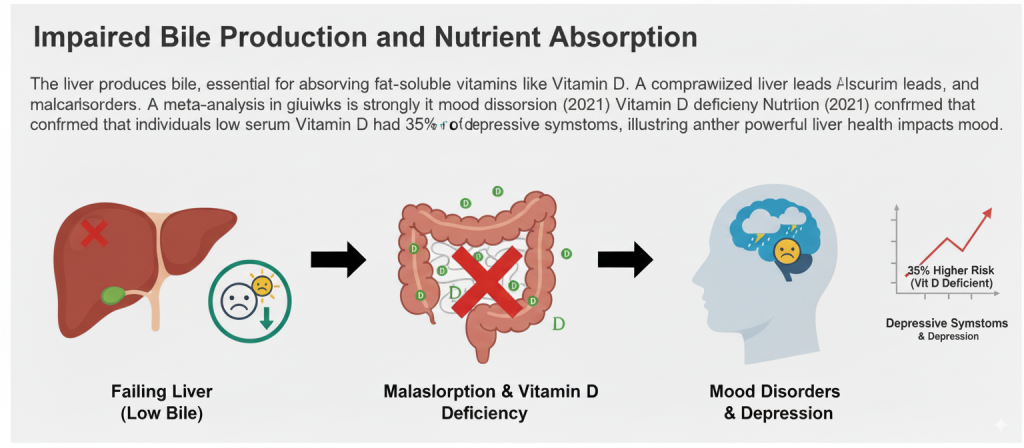
Impaired Bile Production and Nutrient Absorption
The liver produces bile, essential for absorbing fat-soluble vitamins like Vitamin D. A compromised liver leads to malabsorption, and Vitamin D deficiency is strongly linked to mood disorders. A meta-analysis in the American Journal of Clinical Nutrition (2021) confirmed that individuals with low serum Vitamin D had a 35% higher risk of depressive symptoms, illustrating another powerful way liver health impacts mood.
How to Identify Liver-Related Mood Changes
Target Population Characteristics: Meet 2 or more of the following:
History of high alcohol consumption or viral hepatitis.
Diagnosis of Non-Alcoholic Fatty Liver Disease (NAFLD), often associated with obesity.
Presence of physical signs such as jaundice, dark urine, or persistent fatigue.
Patients with elevated liver enzymes (ALT/AST) have a significantly higher prevalence of major depressive disorder, as reported in General Hospital Psychiatry (2019).
Diagnostic Methods & Supporting Data:
Liver Function Tests (LFTs): Blood tests for ALT, AST, bilirubin, and albumin.
Ammonia Levels: Blood test to check for a key indicator of HE.
Imaging: Ultrasound or FibroScan to assess liver structure and damage.
Liver Support Strategies:
When mood issues coincide with signs of a strained liver, a proactive approach is crucial. This includes lifestyle changes like eliminating alcohol and reducing processed food intake.
For targeted support, a combination of Milk Thistle (Silymarin) and Turmeric (Curcumin) offers a powerful benefit. Silymarin is a well-researched antioxidant that protects liver cells, while Curcumin is a potent anti-inflammatory agent.
The formulation of BISPIT Hepato-Protect Complex is based on this synergy. By protecting liver cells from oxidative stress and reducing systemic inflammation, it helps restore the liver’s capacity to detoxify ammonia, balance hormones, and support proper nutrient absorption. Addressing liver dysfunction can break the cycle of toxicity, leading to marked improvements in both cognitive function and emotional stability.
Data Sources:
Journal of Hepatology 2018;69(3):551-563
Metabolism: Clinical and Experimental 2020;112:154360
American Journal of Clinical Nutrition 2021;113(5):1101-1112
General Hospital Psychiatry 2019;58:24-30
